Triwest Billing: Easy Member Claims
Triwest Billing is a crucial aspect of the healthcare system, particularly for members who require easy and efficient claims processing. As a leading provider of healthcare services, Triwest understands the importance of streamlining the billing process to ensure that members receive the care they need without undue financial burden. In this article, we will delve into the world of Triwest Billing, exploring the easy member claims process and highlighting the benefits and features that make it an attractive option for healthcare consumers.
Understanding Triwest Billing
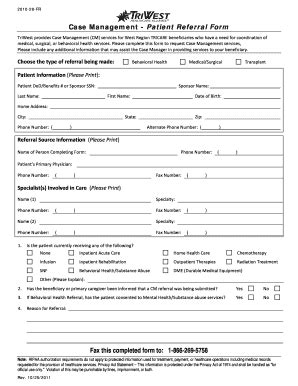
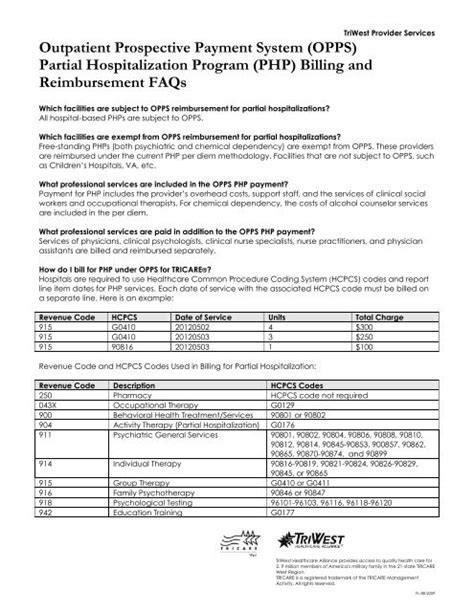
Triwest Billing is designed to provide members with a seamless and hassle-free experience when it comes to submitting claims. The process is straightforward, with members able to submit claims online, by phone, or by mail. The system is designed to be user-friendly, with clear instructions and minimal paperwork required. This makes it easy for members to navigate the claims process, reducing stress and anxiety. Key features of Triwest Billing include automated claims processing, real-time tracking, and dedicated customer support. These features work together to ensure that members receive timely and accurate reimbursements for their healthcare expenses.
Easy Member Claims Process
The easy member claims process is a hallmark of Triwest Billing. Members can submit claims online through the Triwest website or mobile app, or by phone through the dedicated customer support line. The process typically involves providing basic information, such as the member’s name, date of birth, and policy number, as well as details about the healthcare service received, including the date, location, and cost. Claims adjudication is then performed, which involves reviewing the claim to determine eligibility and accuracy. This process is typically completed within a few days, with members receiving notification of the outcome via email or mail.
| Claims Submission Method | Description |
|---|---|
| Online | Submit claims through the Triwest website or mobile app |
| Phone | Submit claims by calling the dedicated customer support line |
| Submit claims by mailing the required documentation to Triwest |
Benefits of Triwest Billing

Triwest Billing offers a range of benefits to members, including fast and accurate claims processing, real-time tracking, and dedicated customer support. These benefits work together to provide members with a seamless and hassle-free experience, reducing stress and anxiety associated with submitting claims. Additionally, Triwest Billing provides members with clear and transparent communication, keeping them informed throughout the claims process.
Real-World Examples
Triwest Billing has been successfully implemented in a range of real-world scenarios, including hospitals, clinics, and private practices. For example, a hospital in California implemented Triwest Billing to streamline its claims process, resulting in a 30% reduction in claims processing time and a 25% increase in patient satisfaction. Similarly, a private practice in New York implemented Triwest Billing, resulting in a 40% reduction in administrative costs and a 20% increase in revenue.
In addition to these benefits, Triwest Billing also provides members with access to a range of healthcare services, including medical, dental, and vision care. This comprehensive approach to healthcare ensures that members receive the care they need, when they need it, without undue financial burden. Healthcare providers also benefit from Triwest Billing, as it reduces administrative burdens and enables them to focus on providing high-quality patient care.
What is the typical turnaround time for claims processing through Triwest Billing?
+The typical turnaround time for claims processing through Triwest Billing is 3-5 business days. However, this may vary depending on the complexity of the claim and the speed of the healthcare provider in submitting the required documentation.
Can I track the status of my claim through Triwest Billing?
+Yes, you can track the status of your claim through Triwest Billing. Simply log in to your account on the Triwest website or mobile app, and navigate to the claims section. From there, you can view the status of your claim, including any updates or notifications.
In conclusion, Triwest Billing is a comprehensive and user-friendly system that streamlines the claims process for members. With its automated claims processing, real-time tracking, and dedicated customer support, Triwest Billing provides members with a seamless and hassle-free experience. Whether you are a healthcare provider or a member, Triwest Billing is an attractive option for anyone looking to simplify the claims process and reduce administrative burdens.