Stereotactic Brain Biopsy: A Comprehensive Guide To Precision Diagnosis
In the ever-evolving field of medical diagnostics, stereotactic brain biopsy has emerged as a revolutionary technique, offering precision and accuracy in the diagnosis of various brain conditions. This procedure, a minimally invasive approach, has transformed the way neurologists and neurosurgeons approach complex brain disorders, providing invaluable insights for treatment planning.
With an increasing focus on personalized medicine, the demand for precise and targeted diagnostic methods has never been more critical. Stereotactic brain biopsy stands as a testament to this evolution, offering a less invasive alternative to traditional open brain surgery. In this comprehensive guide, we will delve into the intricacies of this procedure, exploring its history, benefits, techniques, and its pivotal role in modern neurological care.
The Evolution of Stereotactic Brain Biopsy: A Historical Perspective
The concept of stereotactic surgery, which forms the basis of stereotactic brain biopsy, dates back to the early 20th century. However, it was in the 1940s that the technique began to be refined and applied to brain surgery. Dr. Victor Horsley, a British neurosurgeon, is often credited with pioneering the use of stereotactic techniques for brain surgery, developing a frame-based system to guide surgical interventions.
Over the years, stereotactic surgery evolved, with the introduction of computed tomography (CT) and magnetic resonance imaging (MRI) in the 1970s and 1980s, respectively, revolutionizing the field. These imaging modalities allowed for more precise targeting of brain lesions, enhancing the accuracy and safety of stereotactic procedures. The development of frameless stereotaxy further improved the accessibility and flexibility of these procedures, making them more widely applicable.
Understanding Stereotactic Brain Biopsy: An Overview

Stereotactic brain biopsy is a surgical procedure used to obtain a small sample of brain tissue for diagnostic purposes. This procedure is typically employed when there is a need to confirm the presence of a brain lesion, such as a tumor, infection, or inflammatory condition. By providing a definitive diagnosis, stereotactic brain biopsy guides treatment decisions, ensuring that patients receive the most appropriate and effective care.
The procedure involves the precise insertion of a needle into the brain, guided by advanced imaging techniques such as CT or MRI. This needle is used to extract a small sample of tissue from the suspected lesion. The tissue sample is then sent to a laboratory for analysis, where pathologists examine it under a microscope to determine the nature of the lesion.
Benefits of Stereotactic Brain Biopsy
- Minimally Invasive: Unlike traditional open brain surgery, stereotactic brain biopsy is a minimally invasive procedure. This means it requires only a small incision and causes minimal damage to the surrounding brain tissue, leading to faster recovery times and reduced risk of complications.
- Precision: The use of advanced imaging techniques ensures that the biopsy is targeted precisely at the area of interest, increasing the likelihood of obtaining a diagnostic sample.
- Rapid Diagnosis: Stereotactic brain biopsy provides a quick and accurate diagnosis, allowing for timely treatment planning. This is particularly crucial in cases where prompt intervention can significantly impact patient outcomes.
- Safety: With advancements in imaging and surgical techniques, stereotactic brain biopsy has become a highly safe procedure. The precise targeting and real-time monitoring during the procedure minimize the risk of damage to critical brain structures.
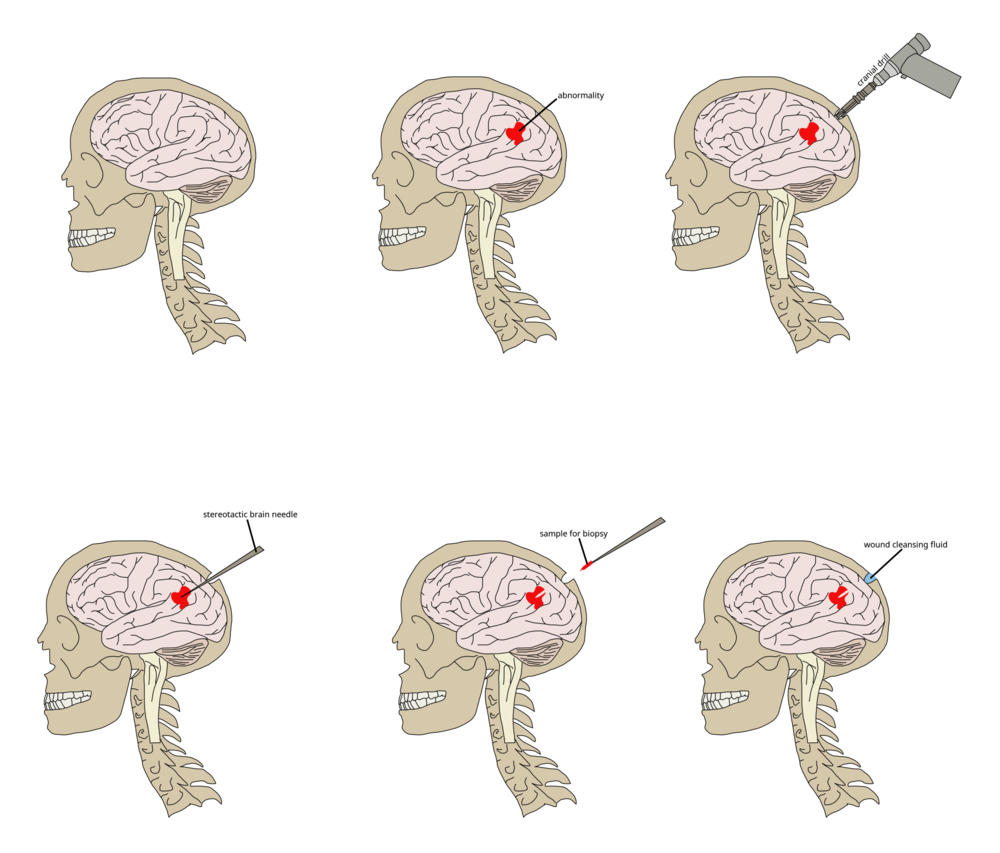
The Procedure: A Step-by-Step Guide
Stereotactic brain biopsy is a highly specialized procedure, typically performed by a team of neurosurgeons, neurologists, and radiologists. Here is a simplified step-by-step breakdown of the process:
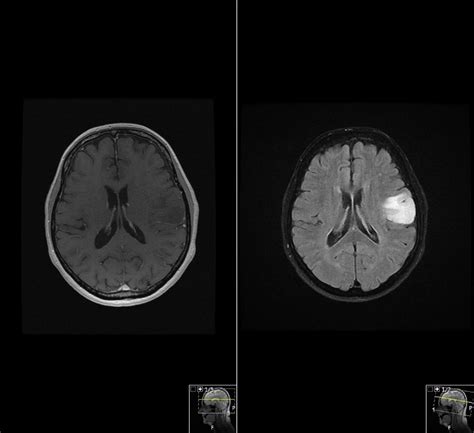
- Planning and Imaging: The first step involves obtaining detailed imaging of the brain using CT or MRI scans. These images are used to plan the biopsy, identifying the precise location of the lesion and determining the optimal trajectory for the needle.
- Anesthesia and Patient Preparation: The patient is typically placed under local anesthesia, with sedation to ensure comfort and minimize movement during the procedure. The scalp and skull are then cleaned and prepared for surgery.
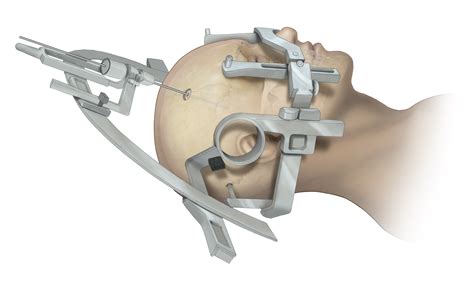
- Frame Placement (for Frame-Based Biopsies): In some cases, a stereotactic frame is attached to the patient's head to provide a fixed reference point for the biopsy. This frame is precisely positioned using the imaging data and secured to the skull using pins.
- Needle Insertion: Using the imaging data and the stereotactic frame (if used), the surgeon inserts a fine needle into the brain, guided by real-time imaging. The needle is advanced to the target location, ensuring precise placement.
- Tissue Sampling: Once the needle is in position, a small sample of brain tissue is extracted. This is done by applying suction or using a specialized biopsy needle with a cutting mechanism. The sample is then sent for immediate analysis.
- Post-Biopsy Imaging: After the biopsy, additional imaging may be performed to confirm the accuracy of the procedure and to assess for any potential complications.
- Wound Closure and Recovery: The small incision is closed, and the patient is monitored for a short period. Most patients can expect to be discharged within a day or two, with minimal discomfort and a rapid recovery.
Technical Specifications and Equipment
The success of stereotactic brain biopsy relies on advanced imaging and surgical equipment. Here are some key components:
- Imaging Modalities: CT and MRI scanners are essential for obtaining detailed brain images, which are crucial for planning and performing the biopsy.
- Stereotactic Frames (for Frame-Based Biopsies): These frames provide a fixed reference point, ensuring precise needle placement. They are typically made of lightweight, durable materials and are designed for patient comfort.
- Biopsy Needles: Fine, specialized needles are used to extract the tissue sample. These needles are designed to minimize damage to the surrounding tissue and are often equipped with cutting mechanisms or suction devices.
- Neurosurgical Microscopes: These high-powered microscopes allow surgeons to visualize the brain tissue during the procedure, ensuring precision and accuracy.
Performance Analysis: Success Rates and Patient Outcomes
Stereotactic brain biopsy has consistently demonstrated high success rates and favorable patient outcomes. Numerous studies have reported diagnostic accuracy rates of over 90%, with minimal complications.
One of the key advantages of stereotactic brain biopsy is its ability to provide a definitive diagnosis, leading to more effective and targeted treatment plans. This is particularly beneficial in cases where a precise diagnosis is crucial for determining the most appropriate treatment approach, such as in the case of brain tumors or inflammatory brain disorders.
Additionally, the minimally invasive nature of the procedure contributes to its success. Patients typically experience shorter hospital stays, faster recovery times, and reduced risk of complications compared to traditional open brain surgery. This translates to improved patient satisfaction and quality of life, making stereotactic brain biopsy a preferred diagnostic option in many cases.
Case Studies: Real-World Applications
To illustrate the impact of stereotactic brain biopsy, let’s explore a couple of real-world case studies:
- Case 1: Brain Tumor Diagnosis - A 45-year-old patient presented with persistent headaches and seizures. MRI scans revealed a suspicious lesion in the frontal lobe. A stereotactic brain biopsy was performed, confirming the presence of a low-grade glioma. This precise diagnosis allowed for targeted treatment planning, including surgical resection and adjuvant therapy, leading to a successful outcome.
- Case 2: Inflammatory Brain Disorder - A 32-year-old patient experienced progressive cognitive decline and memory loss. Initial imaging suggested an inflammatory condition. A stereotactic brain biopsy was performed, revealing the presence of an autoimmune encephalitis. This diagnosis led to prompt immunotherapy, resulting in a significant improvement in the patient's symptoms and cognitive function.
Future Implications and Innovations
As medical technology continues to advance, stereotactic brain biopsy is poised to play an even more significant role in neurological care. Here are some future implications and potential innovations:
- Robotic-Assisted Biopsies: The integration of robotic technology into stereotactic brain biopsy procedures could enhance precision and reduce the risk of human error. Robotic systems can provide real-time feedback and adjust needle trajectories based on intraoperative imaging, further improving accuracy.
- Advanced Imaging Techniques: The development of more advanced imaging modalities, such as functional MRI and PET scans, could provide even more detailed information about brain lesions. This could lead to more precise targeting of biopsies and improved diagnostic accuracy.
- Minimally Invasive Biopsy Devices: Ongoing research and development are focused on creating even smaller and more flexible biopsy devices. These devices could potentially be inserted through natural openings, such as the nose, further reducing the invasiveness of the procedure.
- Artificial Intelligence (AI) Integration: AI algorithms could be used to analyze imaging data and provide real-time feedback during stereotactic brain biopsies. This could enhance the speed and accuracy of diagnosis, particularly in complex cases.
Conclusion: The Future of Neurological Diagnostics
Stereotactic brain biopsy represents a significant advancement in the field of neurological diagnostics, offering precision, accuracy, and minimally invasive diagnosis. Its ability to provide a definitive diagnosis for a range of brain conditions has revolutionized treatment planning, leading to improved patient outcomes and quality of life.
As we look to the future, the continued evolution of stereotactic brain biopsy, coupled with advancements in imaging, robotics, and AI, promises even more precise and effective diagnostic capabilities. This procedure stands as a testament to the power of medical innovation, shaping the future of neurological care and offering hope to patients facing complex brain disorders.
How does stereotactic brain biopsy compare to traditional open brain surgery in terms of recovery time and complications?
+Stereotactic brain biopsy is a minimally invasive procedure, which means it requires only a small incision and causes minimal damage to the surrounding brain tissue. As a result, patients typically experience shorter hospital stays, faster recovery times, and reduced risk of complications compared to traditional open brain surgery. This is due to the precision and accuracy of the stereotactic technique, which minimizes the risk of damage to critical brain structures.
What are the potential risks and complications associated with stereotactic brain biopsy?
+While stereotactic brain biopsy is generally considered a safe procedure, like any surgical intervention, it carries some risks. These include the potential for infection, bleeding, and damage to surrounding brain tissue. However, with advancements in imaging and surgical techniques, the risk of complications has significantly decreased. It is important to discuss these potential risks with your healthcare provider prior to undergoing the procedure.
How long does the entire stereotactic brain biopsy process take, from planning to recovery?
+The entire process, from initial planning and imaging to recovery, typically takes a few days. The actual biopsy procedure itself is usually completed within a few hours. However, the time required for planning, anesthesia, and post-biopsy monitoring can vary depending on the specific case and the patient’s individual needs. Most patients can expect to be discharged within a day or two after the procedure, with minimal discomfort and a rapid recovery.


