Emergent Bladder: Symptoms And Treatment Options
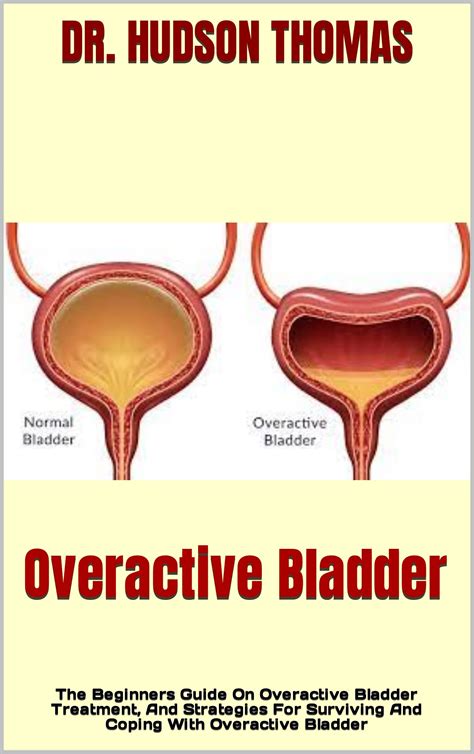
The emergent bladder, also known as overactive bladder (OAB), is a condition characterized by a sudden and intense urge to urinate, often accompanied by involuntary loss of urine. This condition can significantly impact an individual's quality of life, causing embarrassment, anxiety, and disruption to daily activities. Understanding the symptoms and treatment options for emergent bladder is crucial for effective management and improved quality of life.
Causes and Risk Factors

The exact cause of emergent bladder is often unclear, but several factors can contribute to its development. Neurological disorders, such as multiple sclerosis, Parkinson’s disease, and stroke, can damage the nerves that control the bladder, leading to OAB symptoms. Urinary tract infections (UTIs) and bladder stones can also irritate the bladder and cause urgency and frequency. Additionally, hormonal changes during menopause can lead to a decline in estrogen levels, which can contribute to OAB symptoms in women.
Symptoms of Emergent Bladder
The primary symptoms of emergent bladder include:
- Sudden and intense urge to urinate
- Urinary frequency, defined as urinating more than eight times in 24 hours
- Urinary urgency, defined as a sudden and compelling need to urinate
- Nocturia, defined as waking up multiple times at night to urinate
- Urinary incontinence, defined as the involuntary loss of urine
These symptoms can vary in severity and impact daily life, making it essential to seek medical attention for proper diagnosis and treatment.
Treatment Options for Emergent Bladder

Treatment for emergent bladder typically involves a combination of lifestyle modifications, behavioral therapies, and medications. Lifestyle modifications include:
- Fluid management: avoiding caffeinated and carbonated beverages, and drinking water in moderation
- Dietary changes: avoiding spicy, acidic, or sugary foods that can irritate the bladder
- Weight management: maintaining a healthy weight to reduce pressure on the bladder
- Pelvic floor exercises: strengthening the muscles that support the bladder and urethra
Behavioral therapies include:
- Bladder training: gradually increasing the time between urinations to improve bladder control
- Pelvic floor physical therapy: exercises and techniques to strengthen the pelvic floor muscles
- Biofeedback: using sensors and feedback to become aware of and control pelvic floor muscle contractions
Medications for emergent bladder include:
| Medication | Mechanism of Action |
|---|---|
| Anticholinergics | Block the action of acetylcholine, a neurotransmitter that stimulates bladder contractions |
| Beta-3 adrenergic agonists | Relax the bladder muscle and increase bladder capacity |
| Neuromodulators | Modulate the nerve signals that control bladder function |
These medications can help reduce symptoms of emergent bladder, but may have side effects and interact with other medications.
Advanced Treatment Options
In some cases, advanced treatment options may be necessary to manage emergent bladder symptoms. These include:
- Botulinum toxin injections: injecting botulinum toxin into the bladder muscle to relax it and reduce contractions
- Neuromodulation therapies: using implantable devices or external stimulators to modulate nerve signals and improve bladder function
- Surgery: procedures such as bladder augmentation or sacral neuromodulation to improve bladder function and reduce symptoms
These advanced treatment options should be considered under the guidance of a healthcare provider and after exploring other treatment options.
What is the difference between emergent bladder and overactive bladder?
+Emergent bladder and overactive bladder (OAB) are often used interchangeably, but they refer to the same condition. The term "emergent bladder" is sometimes used to describe the sudden and intense urge to urinate, while "overactive bladder" refers to the broader condition characterized by urinary urgency, frequency, and incontinence.
Can emergent bladder be cured?
+While emergent bladder can be managed and symptoms can be improved, it is often a chronic condition that requires ongoing treatment and lifestyle modifications. In some cases, symptoms may resolve on their own, but it is essential to work with a healthcare provider to develop a personalized treatment plan and improve overall quality of life.
In conclusion, emergent bladder is a complex condition that requires a comprehensive treatment approach. By understanding the causes, symptoms, and treatment options, individuals can work with their healthcare provider to develop a personalized plan to manage symptoms and improve overall quality of life. With the right treatment and lifestyle modifications, it is possible to reduce the impact of emergent bladder and regain control over bladder function.